- BioWorld
- BioWorld MedTech
- BioWorld Asia
- BioWorld Science
- Data Snapshots
- Special reports
- Infographics: Dynamic digital data analysis
- Trump administration impacts
- Biopharma M&A scorecard
- BioWorld 2024 review
- BioWorld MedTech 2024 review
- BioWorld Science 2024 review
- Women's health
- China's GLP-1 landscape
- PFA re-energizes afib market
- China CAR T
- Alzheimer's disease
- Israel
- Rise of obesity
- Radiopharmaceuticals
- Biosimilars
- Aging
- IVDs on the rise
- Coronavirus
- Artificial intelligence
ARTICLES
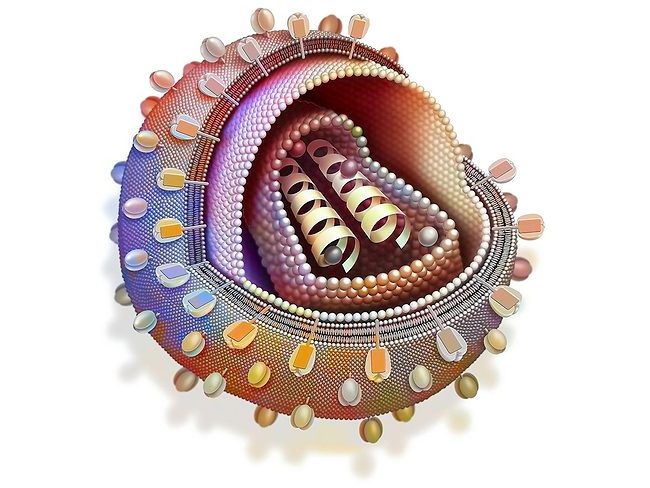
HIV/AIDS
IAS 2024: Seventh HIV cure reported, but broad reach will take other approaches
July 22, 2024
Neurology/psychiatric
ISSCR 2024: Expanding niche definition gives insights into stem cells
July 16, 2024
Musculoskeletal
ISSCR 2024: iPS cell line panels can be isogenic and diverse
July 15, 2024
Neurology/psychiatric
ISSCR 2024: Expanding niche definition gives insights into stem cells
July 12, 2024
Neurology/psychiatric
Studies bring insights into link between glymph system, migraine pain
July 5, 2024
Neurology/psychiatric
EAN 2024: Better diagnoses are shared dream of neurodegeneration researchers
July 1, 2024
Inflammatory
Study gives insight into five inflammatory diseases, and the noncoding genome
June 25, 2024
- BioWorld
- BioWorld MedTech
- BioWorld Asia
- BioWorld Science
- Data Snapshots
- Special reports
- Infographics: Dynamic digital data analysis
- Trump administration impacts
- Biopharma M&A scorecard
- BioWorld 2024 review
- BioWorld MedTech 2024 review
- BioWorld Science 2024 review
- Women's health
- China's GLP-1 landscape
- PFA re-energizes afib market
- China CAR T
- Alzheimer's disease
- Israel
- Rise of obesity
- Radiopharmaceuticals
- Biosimilars
- Aging
- IVDs on the rise
- Coronavirus
- Artificial intelligence