- BioWorld
- BioWorld MedTech
- BioWorld Asia
- BioWorld Science
- Data Snapshots
- Special reports
- Infographics: Dynamic digital data analysis
- Trump administration impacts
- Biopharma M&A scorecard
- BioWorld 2024 review
- BioWorld MedTech 2024 review
- BioWorld Science 2024 review
- Women's health
- China's GLP-1 landscape
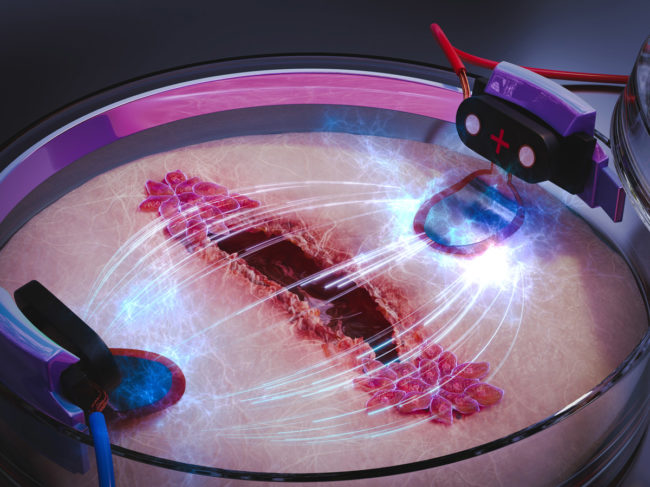
- PFA re-energizes afib market
- China CAR T
- Alzheimer's disease
- Israel
- Rise of obesity
- Radiopharmaceuticals
- Biosimilars
- Aging
- IVDs on the rise
- Coronavirus
- Artificial intelligence
ARTICLES
- BioWorld
- BioWorld MedTech
- BioWorld Asia
- BioWorld Science
- Data Snapshots
- Special reports
- Infographics: Dynamic digital data analysis
- Trump administration impacts
- Biopharma M&A scorecard
- BioWorld 2024 review
- BioWorld MedTech 2024 review
- BioWorld Science 2024 review
- Women's health
- China's GLP-1 landscape
- PFA re-energizes afib market
- China CAR T
- Alzheimer's disease
- Israel
- Rise of obesity
- Radiopharmaceuticals
- Biosimilars
- Aging
- IVDs on the rise
- Coronavirus
- Artificial intelligence