- BioWorld
- BioWorld MedTech
- BioWorld Asia
- BioWorld Science
- Data Snapshots
- Special reports
- Infographics: Dynamic digital data analysis
- Trump administration impacts
- Biopharma M&A scorecard
- BioWorld 2024 review
- BioWorld MedTech 2024 review
- BioWorld Science 2024 review
- Women's health
- China's GLP-1 landscape
- PFA re-energizes afib market
- China CAR T
- Alzheimer's disease
- Israel
- Rise of obesity
- Radiopharmaceuticals
- Biosimilars
- Aging
- IVDs on the rise
- Coronavirus
- Artificial intelligence
ARTICLES
2023 Med Tech Conference
FDA’s Shuren says agency decidedly moving away from up-or-down vote at advisory hearings
Oct. 12, 2023
By Mark McCarty
2023 Med Tech Conference
EU’s notified body dilemma easing, but competent authorities continue to muddle the picture
Oct. 11, 2023
By Mark McCarty
2023 Med Tech Conference
PCCP concept at risk of being subsumed in debate over artificial intelligence
Oct. 10, 2023
By Mark McCarty
2023 Med Tech Conference
Advamed’s Whitaker more bullish on VALID Act in light of FDA draft rule for LDTs
Oct. 10, 2023
By Mark McCarty
2023 Med Tech Conference
Congress seen as having leeway to bring LDT user fees on board midstream in MDUFA VI
Oct. 9, 2023
By Mark McCarty
ASTRO 2023
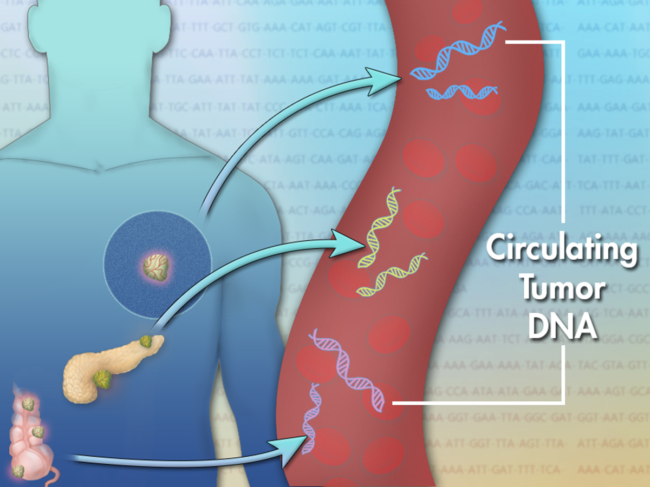
Study suggests that circulating tumor DNA is predictive of response to therapy in NSCLC
Oct. 4, 2023
By Mark McCarty
- BioWorld
- BioWorld MedTech
- BioWorld Asia
- BioWorld Science
- Data Snapshots
- Special reports
- Infographics: Dynamic digital data analysis
- Trump administration impacts
- Biopharma M&A scorecard
- BioWorld 2024 review
- BioWorld MedTech 2024 review
- BioWorld Science 2024 review
- Women's health
- China's GLP-1 landscape
- PFA re-energizes afib market
- China CAR T
- Alzheimer's disease
- Israel
- Rise of obesity
- Radiopharmaceuticals
- Biosimilars
- Aging
- IVDs on the rise
- Coronavirus
- Artificial intelligence