- BioWorld
- BioWorld MedTech
- BioWorld Asia
- BioWorld Science
- Data Snapshots
- Special reports
- Infographics: Dynamic digital data analysis
- Trump administration impacts
- Biopharma M&A scorecard
- BioWorld 2024 review
- BioWorld MedTech 2024 review
- BioWorld Science 2024 review
- Women's health
- China's GLP-1 landscape
- PFA re-energizes afib market
- China CAR T
- Alzheimer's disease
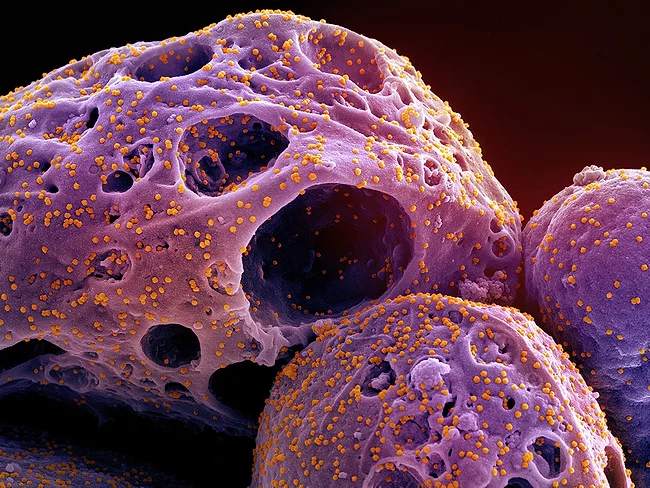
- Coronavirus
- More reports can be found here
ARTICLES
Neurology/Psychiatric
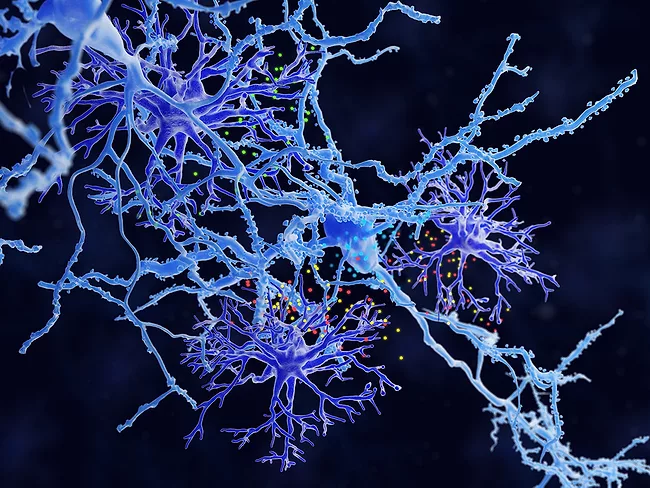
Brain maps uncover individual differences in psychiatric disorders
Aug. 18, 2023
Gastrointestinal
Gut enzyme inhibitor could reduce inflammatory bowel disease symptoms
Aug. 16, 2023
Infection
Viral alteration of mitochondrial function may trigger severe COVID-19
Aug. 14, 2023
Immuno-oncology
At first ASGCT Immuno-oncology meeting, ways to build better T cells
Aug. 3, 2023
Cancer
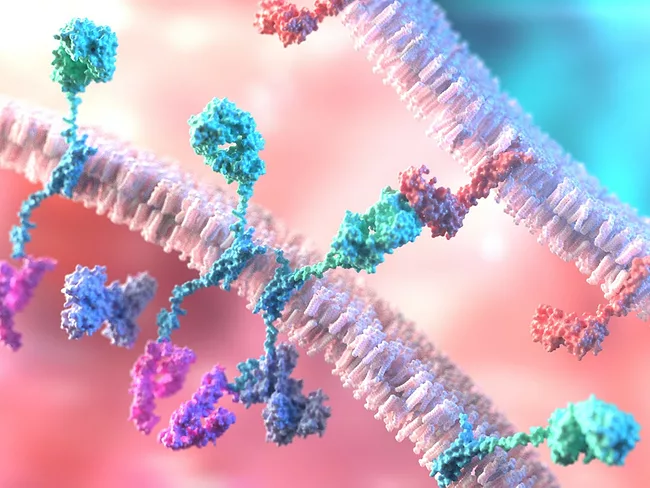
H. pylori induces stomach cancer by disrupting stem cell marching orders
July 28, 2023
- BioWorld
- BioWorld MedTech
- BioWorld Asia
- BioWorld Science
- Data Snapshots
- Special reports
- Infographics: Dynamic digital data analysis
- Trump administration impacts
- Biopharma M&A scorecard
- BioWorld 2024 review
- BioWorld MedTech 2024 review
- BioWorld Science 2024 review
- Women's health
- China's GLP-1 landscape
- PFA re-energizes afib market
- China CAR T
- Alzheimer's disease
- Coronavirus
- More reports can be found here